Gabapentin is a prescription medicine used to treat nerve pain (such as post-herpetic neuralgia after shingles and other peripheral neuropathic pain) and to help control partial-onset seizures as add-on therapy. Many countries also use brand-specific extended-release versions for post-herpetic neuralgia or restless legs syndrome (RLS). Gabapentin is not an opioid and not an NSAID.
In this plain-English guide, you’ll learn what gabapentin is, how it works, when doctors prescribe it, exactly how to take it, possible side effects, key safety tips (breathing risk with other sedatives, driving caution, kidney dosing), and answers to the most-searched questions.
Quick disclaimer: This article is for education only and not a substitute for professional medical advice. Always follow your prescriber’s instructions and the patient leaflet for your exact brand and country.
What Is Gabapentin?
Gabapentin is an antiepileptic/antineuralgic medicine. It’s available as:
- Immediate-release (IR): capsules, tablets, oral solution (common strengths: 100 mg, 300 mg, 400 mg, 600 mg, 800 mg).
- Extended-release (ER) gabapentin (brand specific): tablets taken once daily with an evening meal for certain pain conditions.
- Gabapentin enacarbil (a prodrug; brand specific): designed for RLS and post-herpetic neuralgia in some regions.
These forms are not interchangeable milligram-for-milligram. Use exactly the product prescribed.
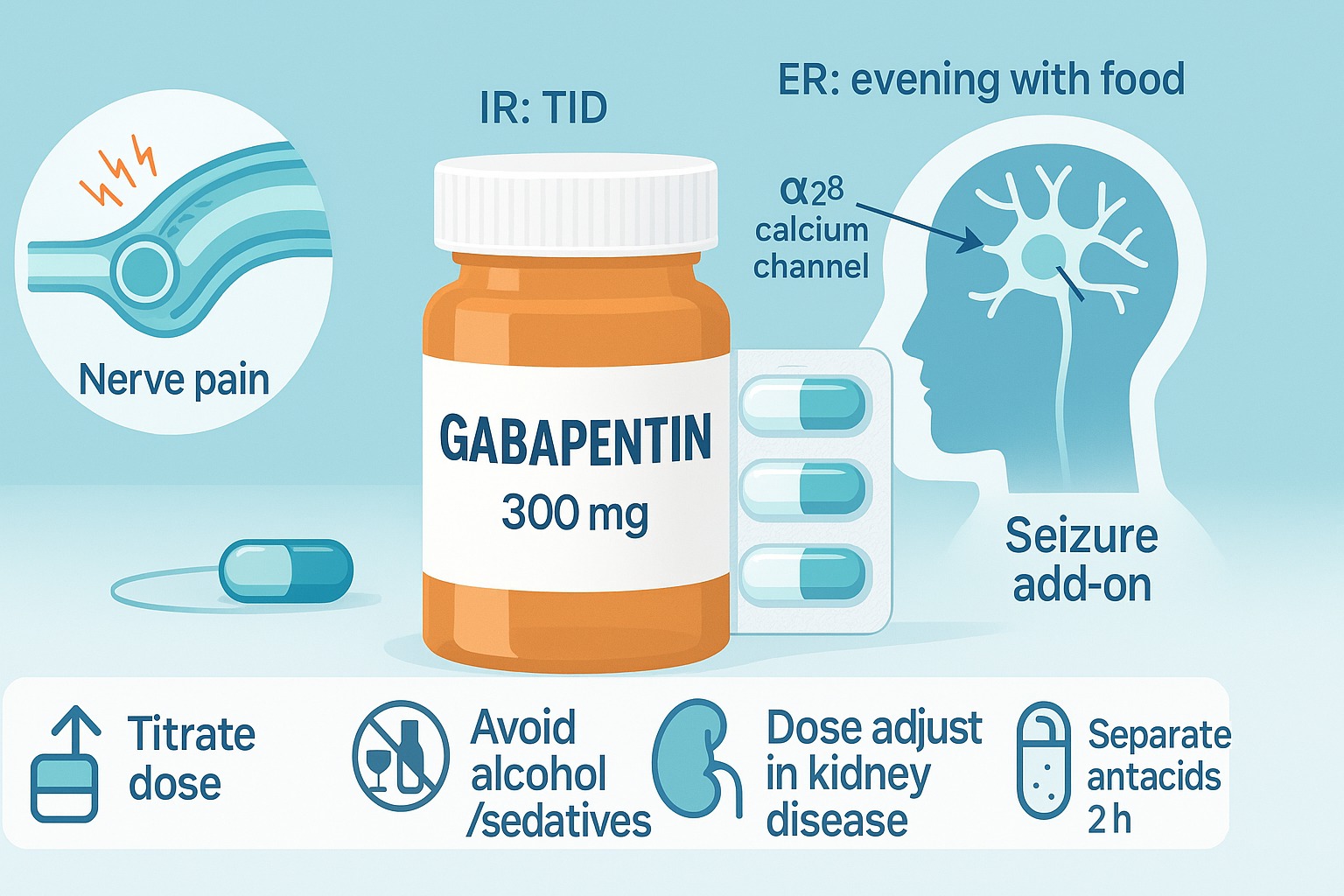
How Does Gabapentin Work?
Gabapentin is structurally similar to GABA but doesn’t act directly on GABA receptors. Instead, it binds to the α2δ subunit of voltage-gated calcium channels in the nervous system. This dampens release of excitatory neurotransmitters, helping calm overactive pain signals and stabilize electrical activity that can trigger seizures.
Common Uses of Gabapentin
- Peripheral neuropathic pain, including post-herpetic neuralgia (PHN) after shingles; often used for diabetic neuropathy and other nerve pain as directed by clinicians.
- Adjunct treatment for partial-onset seizures in adults and children (age cutoffs vary by country—commonly ≥3 years for IR).
- Restless legs syndrome (RLS): certain extended-release/prodrug brands are approved in some regions.
Your doctor or pharmacist will match the formulation and dose to your condition.
Gabapentin Dosage & Administration
Doses vary with condition, age, kidney function, and product. Always follow your exact prescription.
Adults – Immediate-Release (IR)
Peripheral neuropathic pain (e.g., PHN)
- Typical titration:
- Day 1: 300 mg once
- Day 2: 300 mg twice daily
- Day 3: 300 mg three times daily
- Maintenance: 900–1,800 mg/day in 3 divided doses (some patients up to 3,600 mg/day if tolerated).
Partial-onset seizures (add-on therapy)
- Often 300 mg three times daily to start or after a brief titration.
- Usual range: 900–1,800 mg/day in 3 divided doses (max 3,600 mg/day in some adults).
Pediatric (IR) – Seizure Add-On (typical guidance)
- 3–11 years: start around 10–15 mg/kg/day, then titrate over several days to 25–35 mg/kg/day divided TID.
- ≥12 years: adult-like dosing.
Extended-Release Gabapentin / Gabapentin Enacarbil
- Use brand-specific schedules (e.g., once daily with the evening meal for certain tablets; for some RLS products, early evening dosing).
- Do not crush, split, or substitute with IR—these are not equivalent.
Practical Tips
- Take IR gabapentin three times daily (morning/afternoon/bedtime) for steady levels.
- Antacids with aluminum/magnesium can reduce absorption—separate by ≥2 hours.
- If you miss a dose, take it when remembered unless it’s close to the next; don’t double.
- Kidney disease: doses must be reduced; your prescriber will adjust using your eGFR/CrCl.
- Stopping: taper gradually under medical guidance to avoid withdrawal symptoms or rebound seizures.
Side Effects of Gabapentin
Most are dose-related and improve as your body adjusts.
Common
- Dizziness and sleepiness
- Coordination problems/ataxia, tremor
- Swelling in legs/feet, weight gain
- Fatigue, blurred vision, dry mouth
- Nausea, constipation or diarrhea
Less common but important
- Mood changes, depression, irritability; rare suicidal thoughts (a class warning for antiepileptics)
- Severe allergic reaction or DRESS (fever, rash, swollen glands, facial swelling—seek urgent care)
- Breathing problems—risk is higher if you have COPD, are elderly, or combine with opioids/benzodiazepines/alcohol
- Angioedema (swelling of face, lips, tongue—emergency)
Warnings & Precautions
- CNS depression & driving: Gabapentin can impair alertness. Don’t drive or operate machinery until you know your response.
- Opioids, benzodiazepines, alcohol, sleep meds: Combining increases sedation and respiratory depression risk—use only if your prescriber says it’s safe.
- Kidney function: Requires dose adjustment.
- Misuse potential: Some regions classify gabapentin as a controlled medicine—use only as prescribed.
- Pregnancy & breastfeeding: Discuss risks/benefits. Limited human data; gabapentin appears in breast milk—monitor infants for drowsiness or poor feeding.
- Older adults & fall risk: Start low, go slow.
Drug & Product Interactions
- Aluminum/magnesium antacids: Lower gabapentin absorption; separate by at least 2 hours.
- Opioids (e.g., morphine, oxycodone): May increase gabapentin levels and depress breathing—close monitoring required.
- CNS depressants (benzodiazepines, sedating antihistamines, alcohol): additive sedation.
- Herbal products with sedative effects (kava, valerian): caution.
- Vaccines & routine meds: usually compatible, but always share your complete medication list.
Gabapentin vs Other Treatments
- Pregabalin (Lyrica/Lyrica CR): Similar mechanism; more predictable absorption and often faster onset, but typically higher cost and controlled status in many countries. Some patients respond better to one vs the other.
- Antidepressants for nerve pain (e.g., duloxetine, amitriptyline): Strong options; may cause dry mouth, constipation, or sleepiness—choice depends on comorbidities.
- Carbamazepine/oxcarbazepine: Preferred for trigeminal neuralgia; more lab monitoring and interactions.
- Topicals (lidocaine patches, capsaicin) and non-drug therapies (physical therapy, sleep hygiene, TENS) can be added.
Cost & “Over-the-Counter” Status
- Status: Prescription-only (Rx) in the US, UK, Canada, Australia, and Europe.
- Cost: Widely available as generic, often inexpensive; ER/prodrug brands are pricier. Discount programs and national health systems may reduce cost.
Special Section: Immediate-Release vs Extended-Release vs Prodrug
- Immediate-Release (IR) Gabapentin
- Flexible dosing; typically TID.
- Useful for both nerve pain and seizure add-on.
- Extended-Release (ER) Gabapentin
- Once-daily evening dosing for certain pain indications.
- Must be taken with food and swallowed whole.
- Gabapentin Enacarbil (Prodrug)
- Designed for steady absorption; approved in some regions for RLS and PHN.
- Dosing and timing are brand-specific (often early evening for RLS).
- Not interchangeable with IR/ER gabapentin on a mg-to-mg basis.
Proper Care With Gabapentin
Before starting
- Share your full medication list (including OTCs, sleep meds, alcohol use) and medical history (lungs, kidneys, mood).
- Ask which formulation you are receiving and how it differs from other versions.
During treatment
- Take doses consistently; set reminders for TID schedules.
- Avoid alcohol or sedatives unless cleared by your prescriber.
- Stand up slowly to reduce dizziness/fall risk.
- Keep a symptom & side-effect diary (pain scores, sleep, mood).
When to call urgently
- Trouble breathing, severe drowsiness, bluish lips/skin
- Swelling of face/lips/tongue, widespread rash or fever
- New or worsening depression, anxiety, or suicidal thoughts
Frequently Asked Questions (FAQs)
1) How long until gabapentin helps nerve pain?
Some people improve within 1–2 weeks as the dose rises; full benefit may take several weeks at a stable dose.
2) Will it make me sleepy?
Drowsiness and dizziness are common early on. They often lessen after a few days. Avoid driving until you know your reaction.
3) Can I take it just at night?
For IR, pain control usually needs 3 daily doses. Your prescriber may adjust timing if nights are worst.
4) What if I miss a dose?
Take it when you remember unless it’s near the next dose. Do not double.
5) Can I drink alcohol?
Best to avoid or limit it—alcohol adds to sedation and breathing risk, especially with higher doses or other sedatives.
6) Is it addictive?
Gabapentin isn’t an opioid, but misuse can occur. Use exactly as prescribed and never share your medicine.
7) Can I stop suddenly?
No. Taper gradually with your prescriber to avoid withdrawal symptoms or seizure risk in susceptible people.
8) Does food matter?
IR can be taken with or without food. Some ER products must be taken with the evening meal—follow your brand’s directions.
9) Is it safe in pregnancy or breastfeeding?
Talk with your clinician. Data are limited; benefits and risks must be weighed. Infants exposed via breast milk should be watched for excess sleepiness.
10) What strength should I start with?
Many adults start at 300 mg and titrate. Your clinician will pick a plan based on your condition and kidney function.
11) Can antacids affect it?
Yes—aluminum/magnesium antacids lower absorption. Separate by at least 2 hours.
12) What if gabapentin doesn’t help me?
Your prescriber may adjust the dose, switch to pregabalin, or consider duloxetine, TCAs, topical agents, or a multimodal pain plan.
Final Thoughts
Gabapentin can be a useful, non-opioid option for nerve pain and a reliable add-on for certain seizures—when used safely and consistently. Know your exact formulation, follow the titration, avoid alcohol and sedatives, and watch for dizziness or mood changes. Partner with your healthcare professional to tailor the dose and consider supportive therapies (sleep, activity, stress management) for the best long-term results.

Leave a Comment