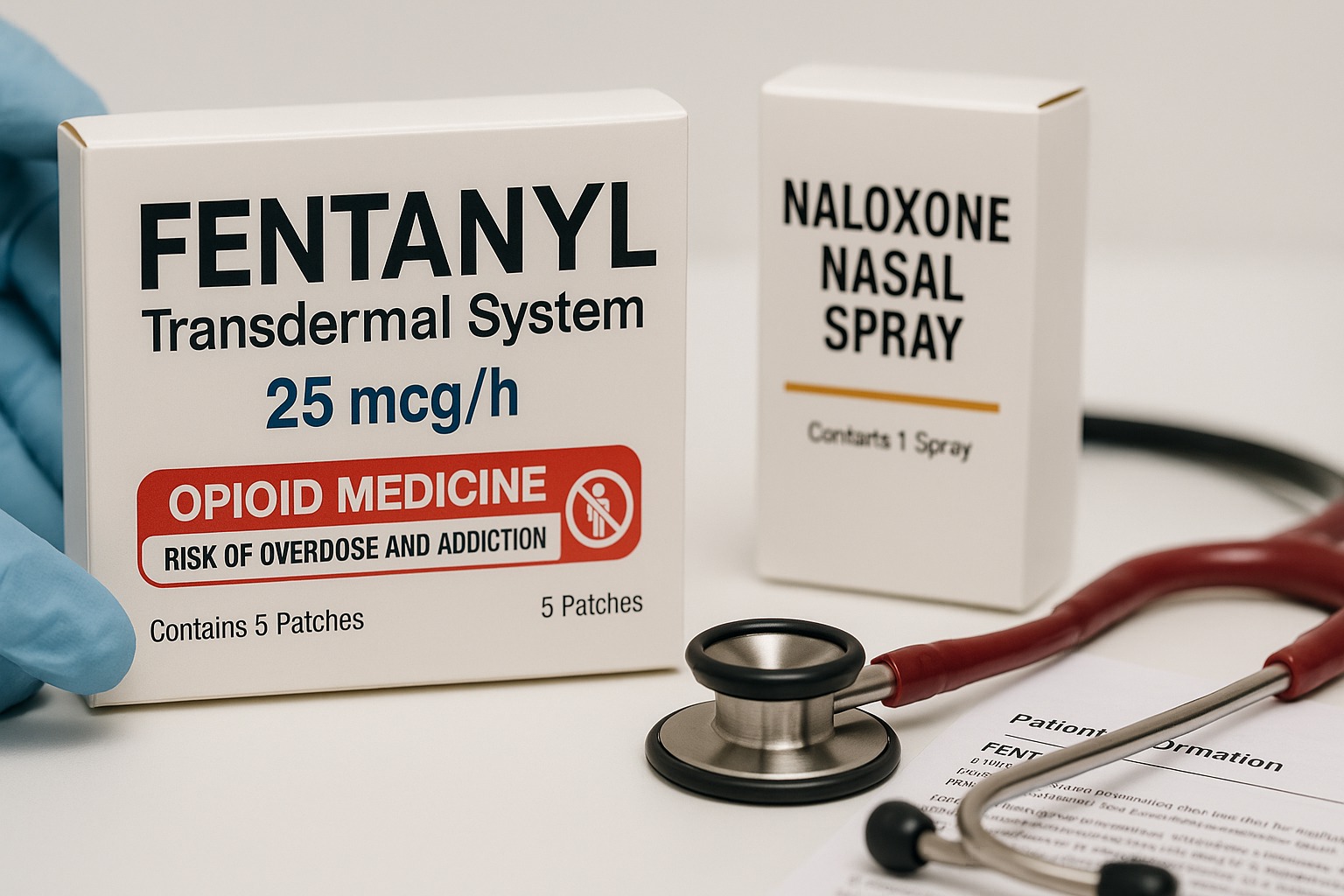
Fentanyl is a strong prescription opioid analgesic used to treat severe pain when other pain medicines are not enough—such as cancer pain, palliative care, or anaesthesia settings. Because fentanyl is 50–100 times stronger than morphine, it carries serious risks and must be used exactly as directed by a qualified clinician.
Education only — not medical advice. Opioids have different brand names, formulations, and regulations across the US, UK, Canada, Australia, and Europe. Always follow your prescriber, pharmacist, and your local Medication Guide/Patient Information Leaflet. Never use fentanyl unless it was prescribed for you.
What Is Fentanyl?
- Class: Potent opioid (μ-opioid receptor agonist)
- Indications (clinician-directed):
- Transdermal patch for opioid-tolerant patients with persistent severe pain (e.g., cancer, palliative care)
- Buccal/lozenge/sublingual products for breakthrough cancer pain in opioid-tolerant adults
- IV/epidural forms used by professionals for anaesthesia or procedural analgesia
- Not for mild, short-term, or occasional pain; not for opioid-naïve patients in most outpatient settings.
High-Alert Safety Warnings (Read First)
- Overdose risk: Even small mistakes can be fatal. Overdose signs include slow or stopped breathing, blue lips/skin, extreme sleepiness, and pinpoint pupils. Call emergency services immediately and use naloxone if available.
- Patch dangers: Heat (fever, heating pads, hot baths/saunas) can release too much medicine. Keep patches flat, secure, and out of children’s reach; fold sticky sides together and dispose per local guidance.
- Interactions that can kill:
- Alcohol, benzodiazepines, sedative-hypnotics, gabapentinoids, or other opioids → severe sedation/respiratory depression
- CYP3A4 inhibitors (e.g., clarithromycin, erythromycin, azole antifungals, ritonavir/cobicistat) → dangerous fentanyl levels
- MAO inhibitors (and within 14 days of stopping) → serotonin & CNS toxicity
- Never cut or chew patches, films, or lozenges; do not inject or use in any way other than prescribed.
- Opioid tolerance requirement: Most community fentanyl products are for patients already taking regular opioids. Starting fentanyl in someone who is opioid-naïve can be fatal.
How Fentanyl Works (simple explanation)
Fentanyl attaches to μ-opioid receptors in the brain and spinal cord, blocking pain signals and often causing sedation. Because it’s lipophilic and very potent, it enters the brain quickly—helpful for severe pain but also the reason it’s high-risk for overdose.
Forms & How They’re Used (overview, no dosing)
Your prescriber determines the dose and product. Do not adjust on your own.
- Transdermal patch (applied every 72 hours in most products): provides a steady release for chronic severe pain in opioid-tolerant adults. Apply to clean, hairless skin on the upper body/arm. Do not expose to heat, and rotate sites to avoid irritation.
- Buccal/sublingual/lozenge (for breakthrough cancer pain): placed inside the cheek or under the tongue to absorb through the mouth lining. Use only the number of doses your clinician allows per day.
- Injectable: used only in hospitals/clinics by trained professionals.
Common Side Effects
- Drowsiness, dizziness, slowed thinking
- Nausea, constipation, dry mouth
- Itching, sweating
- Headache
- Application-site reactions (patch)
Call your clinician urgently for: difficult or slowed breathing, severe sleepiness, confusion, fainting, hallucinations, allergic swelling/rash, or if a child/pet is exposed to a patch or leftover product.
Misuse, Dependence & Withdrawal
- Fentanyl can cause physical dependence and addiction. Use lowest effective dose for the shortest time compatible with your pain plan.
- Do not stop suddenly if you’ve been using it regularly—this can cause withdrawal (restlessness, sweating, stomach cramps, diarrhoea, runny nose, anxiety). Your prescriber will create a slow taper if it’s time to stop.
Safe-Use Checklist (for patients & carers)
- Use exactly as prescribed. No early refills, no sharing.
- Store locked and out of sight—ideally in a lockbox. Keep an inventory count.
- Dispose safely: fold used patches adhesive-to-adhesive; follow local disposal instructions (some regions allow pharmacy take-back or approved disposal pouches).
- Avoid alcohol and sedatives. If you must take a benzodiazepine or sleep medicine, this should be explicitly coordinated by the prescriber.
- Heat precautions (patch): avoid heating pads, electric blankets, saunas/hot tubs; treat fevers quickly and contact your clinician.
- Carry naloxone: Ask your clinician or pharmacist about take-home naloxone for you and your household; ensure everyone knows when and how to use it.
- Driving/operating machinery: Don’t drive until you know how the medicine affects you and your prescriber says it’s safe under your local laws.
- Pregnancy & breastfeeding: Generally not recommended; discuss urgently if you become pregnant. Fentanyl passes into breast milk.
Who Should Not Use Fentanyl?
- Opioid-naïve individuals for outpatient patches or transmucosal products
- People with severe breathing problems (e.g., acute asthma, significant COPD exacerbation) unless in a monitored setting
- Short-term pain situations (post-op, dental, migraine) where safer options exist
- Children unless specifically prescribed by a paediatric specialist for approved indications
(Labels and age cut-offs vary by region—follow your local leaflet.)
Interactions You Must Tell Your Clinician About
- CYP3A4 inhibitors/inducers: macrolide antibiotics, azole antifungals, HIV antivirals, certain seizure medicines, St. John’s wort
- Other CNS depressants: benzodiazepines, Z-drugs (zolpidem etc.), gabapentin/pregabalin, alcohol, antihistamines
- Serotonergic drugs: SSRIs/SNRIs/MAOIs, triptans — monitor for serotonin syndrome (agitation, sweating, fast heart rate, muscle twitching)
Overdose: What Family & Friends Should Know
- Recognise: slow or stopped breathing, bluish lips, unresponsiveness, very small pupils, snoring/gurgling sounds
- Respond immediately:
- Call emergency number (911/999/112 depending on location)
- Give naloxone (spray or injection) if available
- Rescue breathing if trained
- Stay until help arrives; repeat naloxone per instructions if the person does not wake or breathing worsens
- After any overdose, medical evaluation is essential even if the person wakes up—naloxone can wear off before fentanyl does.
FAQs (fast, plain-English answers)
Is fentanyl the same everywhere?
Formulations and brand names differ by country. Safety principles are the same, but indications and dispensing rules vary—follow your local label and prescriber.
Can I shower with a patch?
Yes, brief showers are usually fine. Avoid hot baths/hot tubs/saunas and do not tape extra heat over a patch.
What if a patch falls off?
Follow your leaflet: generally apply a new patch to a different site and note the new time; never “double up” unless your prescriber says so.
How is fentanyl different from morphine or oxycodone?
It’s much more potent and acts quickly. That’s why strict dosing and monitoring are required.
Can I travel with fentanyl?
Carry it in original packaging with your prescription label and a copy of your clinic letter if possible. Some countries have strict import rules—check before travelling.
Key Takeaways
- Fentanyl is a high-alert opioid reserved for severe, ongoing pain under close medical supervision.
- Overdose prevention is the priority: avoid sedatives/alcohol, beware drug interactions, and keep naloxone on hand.
- Patches and transmucosal products are for opioid-tolerant patients only.
- Store locked, dispose safely, and never share your medicine.
- If you or someone you love struggles with opioid use, contact your clinician or local helpline for confidential support and evidence-based treatment options.

Leave a Comment