Quick disclaimer: This article is for education only and isn’t a substitute for professional medical advice. Always follow the plan you and your clinician agree on.
What Is Ebglyss?
Ebglyss (generic name lebrikizumab) is a prescription biologic medicine used to treat moderate to severe atopic dermatitis (eczema). It’s designed for people whose eczema isn’t controlled well enough with moisturizers and topical treatments alone, or who can’t use those treatments. In many regions, Ebglyss is approved for adults and adolescents (12+ years) under the care of a dermatology professional.
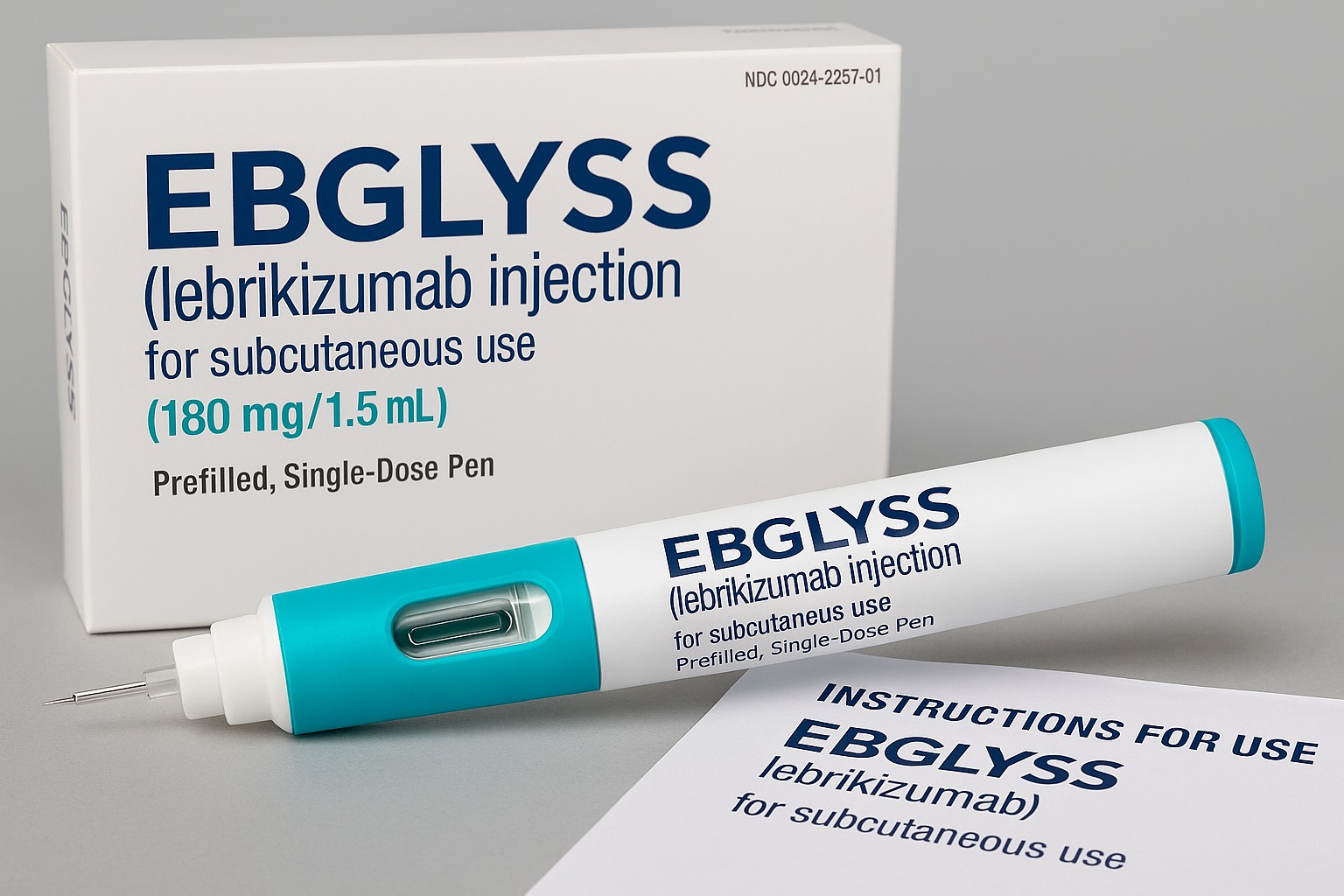
Ebglyss is given as a subcutaneous injection (a shot under the skin) using a prefilled pen or syringe. Many patients learn to self-inject at home after training.
How Ebglyss Works (In Plain English)
Eczema involves an overactive immune response that keeps the skin inflamed, dry, itchy, and prone to infection. A key driver of that inflammation is a signaling protein called interleukin-13 (IL-13). Think of IL-13 as one of the “volume knobs” for allergic skin inflammation.
- Ebglyss is a monoclonal antibody—a lab-made protein—that binds to IL-13 and blocks its ability to send those “itchy/inflamed” signals.
- By turning down IL-13, Ebglyss reduces itch and redness, helps the skin barrier repair, and decreases flares over time.
This targeted mechanism is why Ebglyss is called an immunomodulator. It doesn’t broadly suppress the immune system like older medicines; instead, it focuses on a specific pathway involved in eczema.
Who Might Benefit
Doctors may consider Ebglyss if you:
- Have moderate to severe atopic dermatitis that hasn’t responded adequately to high-quality skin care plus topical steroids or calcineurin inhibitors.
- Need a steroid-sparing option to avoid frequent or long-term use of potent topical steroids.
- Experience frequent flares, intense itch that disrupts sleep and daily activities, or widespread skin involvement.
- Prefer an at-home injectable medicine rather than daily pills or frequent clinic treatments.
Ebglyss is often used with a gentle daily skin-care routine (lukewarm showers, fragrance-free cleansers, thick moisturizers) and, when needed, short courses of topical anti-inflammatories. Many patients still use moisturizers and/or low-to-medium strength steroids for hot spots while Ebglyss handles the background inflammation.
How It’s Given (Dosing & Schedule)
Your prescriber chooses the exact plan based on your age, weight, severity, and response. A common approach in adults and adolescents is:
- Loading phase: A higher starting dose (two injections) to quickly reach effective levels.
- Maintenance: Then one injection every 2 weeks. Some patients who achieve good, stable control may be spaced to every 4 weeks at their clinician’s discretion.
Self-injection happens into fatty tissue, typically the thigh or abdomen (at least 2 inches away from the navel). A caregiver can inject into the back of the upper arm. Rotate sites to help prevent irritation.
Storage: Keep pens/syringes in the refrigerator in the original box. Before injecting, allow the pen to reach room temperature per the instructions (usually ~30 minutes). Do not freeze. Do not shake. Never use if the solution is cloudy, discolored, or has particles.
Missed dose? Take it as soon as you remember unless it’s close to your next scheduled injection. Don’t double up—call your clinic if you’re unsure.
What Results to Expect
Every person is different, but many patients begin to notice less itch in the first few weeks, followed by steadier skin improvement across 2–4 months as the skin barrier heals. Benefits often include:
- Less itch (and better sleep)
- Fewer, milder flares
- Reduced redness and thickness
- Smoother skin and fewer open areas
Sticking with your moisturizer routine and any short-term topical plans your clinician recommends can help speed and stabilize results.
Side Effects and Safety
Most people tolerate Ebglyss well. Side effects are usually mild to moderate and improve over time.
Common effects
- Injection-site reactions (redness, swelling, tenderness, or itch)
- Eye/eyelid problems such as conjunctivitis (pink eye), eye itch, or dryness
- Headache or nasopharyngitis (cold-like symptoms)
Less common but important
- Allergic reactions: hives, swelling, breathing trouble, dizziness, or severe rash—seek urgent medical help.
- Eye inflammation beyond simple irritation (vision changes, pain, sensitivity to light). Contact your clinician if eye symptoms don’t improve with standard care.
- Parasitic (helminth) infections: IL-13 helps your body fight certain parasites. Let your doctor know if you live in or will travel to areas where these infections are common. You may need evaluation and treatment before starting or resuming therapy.
- Infections in general: Tell your doctor if you have a current infection, fever, or are feeling unwell before injecting.
Vaccines: Avoid live vaccines while on Ebglyss. Inactivated vaccines (e.g., flu shots that are not live) are generally fine—check with your clinician first.
Pregnancy & breastfeeding: Human data are limited. If you are pregnant, planning a pregnancy, or nursing, discuss risks and benefits with your prescriber to decide on the safest approach for you and your baby.
Children: In many regions, Ebglyss is approved for 12 years and older; younger ages may vary by country. Pediatric dosing and monitoring are prescriber-directed.
Ebglyss vs. Other Biologics (High-Level Overview)
You may hear Ebglyss mentioned alongside Dupixent® (dupilumab) and Adbry® (tralokinumab). All are injectable biologics for eczema, but there are differences:
- Target:
- Ebglyss and Adbry primarily target IL-13.
- Dupixent blocks the shared receptor for IL-4 and IL-13.
- Schedule: All start with loading doses followed by every-2-weeks injections; some patients maintain control on every-4-weeks spacing (based on clinical judgment and product labeling in your region).
- Eye effects: Conjunctivitis can occur with any of these medicines; your clinician can help manage it promptly.
- Which is “best”? It depends on your skin, other health issues, convenience, insurance coverage, and how you respond. Dermatologists often try one and may switch if control or tolerability isn’t ideal.
Your clinician is the best person to compare options for your specific situation.
Step-by-Step: Self-Injection Tips
Always follow the training you receive from your clinic and the official Instructions for Use in your box. The list below is a general reminder—not a substitute for training.
- Take the pen/syringe out of the fridge and let it warm up to room temperature on a clean surface. Keep it in the original box to protect it from light.
- Check the window—the medicine should be clear to slightly yellow and free of particles.
- Wash your hands. Clean the injection site with an alcohol swab; let it air-dry.
- Choose a site: front of thigh or abdomen (avoid the navel area). If someone is helping, the back of the upper arm is also an option. Rotate sites each time.
- Inject following the device steps (angle, push, hold until the window shows the dose is complete or you hear the end-click—varies by device).
- Dispose of the pen/syringe in an FDA-cleared sharps container. Don’t toss in household trash.
- Moisturize as part of your daily skin routine unless told otherwise.
If you miss a step or aren’t sure whether the dose fully went in, contact your clinic before repeating.
Practical Questions People Ask (FAQs)
1) Is Ebglyss a steroid?
No. It’s a biologic antibody that targets IL-13. It doesn’t thin the skin or cause steroid-type side effects.
2) Can I still use my topical creams?
Often yes. Many people continue moisturizers daily and use short courses of topical steroids or non-steroid anti-inflammatories on trouble spots. Your clinician will tailor the plan.
3) How fast will I feel better?
Some people report less itch in 1–2 weeks; visible skin changes typically build across 4–8+ weeks. Consistency matters.
4) Will I need lab tests?
Routine lab monitoring isn’t usually required with IL-13 blockers, but your clinician may track your overall health or other medications as needed.
5) What about eye side effects?
Tell your clinician promptly if you develop red, itchy, watery eyes or vision changes. Many cases are mild and respond to lubricating drops or prescription eye therapy guided by a dermatologist or eye doctor.
6) Can I stop once my skin looks good?
Eczema is chronic and tends to return if treatment stops. Many patients stay on maintenance dosing long term. If you’re doing great, your clinician may consider spreading out doses—but do this only under medical guidance.
7) How much does it cost?
Prices vary by country, insurance, assistance programs, and pharmacy model. Ask your clinic and pharmacist about manufacturer savings programs and coverage support.
8) Is Ebglyss a cure?
No. It’s a control therapy. When used consistently—alongside smart skin care—it can dramatically reduce symptoms and flares.
Safety Checklist Before Starting
- Share your full medical history, including asthma, eye disease, infections, immune conditions, and any planned surgeries or dental procedures.
- List all medicines and supplements (prescription, OTC, vitamins, herbals).
- Discuss your vaccine history; plan to avoid live vaccines during treatment.
- Tell your clinician if you live in or will travel to areas with parasitic infections.
- If you’re pregnant, planning pregnancy, or breastfeeding, have a risk–benefit conversation first.
Daily Skin Care Still Matters
Even with Ebglyss on board, basic skin care is the backbone of eczema control:
- Use lukewarm showers (5–10 minutes) and fragrance-free cleansers.
- Apply a thick moisturizer (cream or ointment) within 3 minutes after bathing, and at least twice daily on dry areas.
- Wear soft, breathable fabrics; avoid fragrance, harsh detergents, and wool against the skin.
- Identify and minimize personal triggers (sweat, dust mites, stress, certain foods if truly relevant, seasonal changes).
Small habits add up; biologics work best on a well-cared-for skin barrier.
When to Call Your Clinician Urgently
- Signs of a severe allergic reaction: trouble breathing, swelling of face/lips/tongue, widespread hives, feeling faint—call emergency services.
- Severe eye symptoms: significant pain, vision changes, or extreme light sensitivity.
- High fever or serious infection symptoms.
- Skin rapidly worsening or painful, crusted areas that suggest infection.
Ebglyss at a Glance (Quick Recap)
- What it is: A targeted IL-13 blocker (lebrikizumab) for moderate–severe eczema
- How it’s given: Subcutaneous injection—after a loading dose, usually every 2 weeks (some may go every 4 weeks later)
- Benefits: Less itch, fewer flares, healthier skin barrier
- Common side effects: Injection-site reactions, conjunctivitis/eye irritation, mild cold-like symptoms
- Key cautions: No live vaccines, monitor for eye symptoms and infections, consider parasite exposure
- Best results with: Consistent moisturizing, gentle skin care, and good follow-up with your clinician
Final Thoughts
For many people living with moderate to severe eczema, Ebglyss opens the door to steadier control, deeper sleep, and healthier-looking skin—without relying on frequent topical steroids. If you’re considering a biologic, talk with your dermatologist about whether Ebglyss fits your personal history, goals, and lifestyle. Together, you can build a simple, sustainable plan that combines targeted medicine with day-to-day skin care, so you can spend less time itching and more time living.

Leave a Comment