Belbuca is a prescription buccal film used for the long-term management of chronic pain that requires around-the-clock opioid therapy when other options are insufficient. Its active ingredient, buprenorphine, is a partial μ-opioid receptor agonist—a unique opioid that can relieve pain while showing a ceiling to certain effects, such as respiratory depression, compared with full agonists. Belbuca is placed on the inside of the cheek where it slowly dissolves and delivers medicine over time.
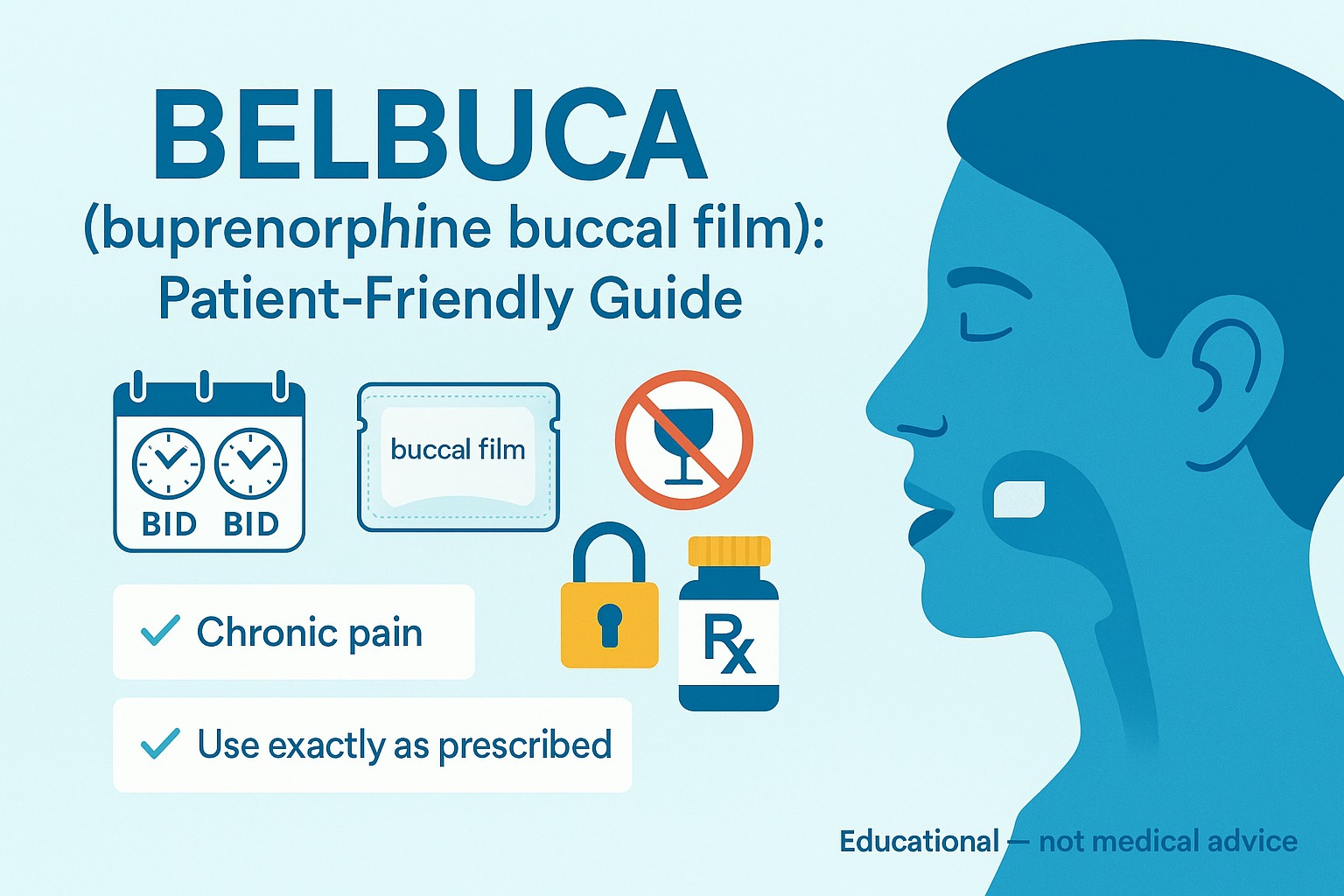
In this clear, patient-friendly guide, you’ll learn what Belbuca is, how it works, when clinicians prescribe it, exactly how to use the film safely, side effects, precautions, drug interactions, cost and generic info, and answers to the internet’s most-searched questions (Belbuca dosage, 150 mcg vs 300 mcg, “Belbuca vs patch,” “Belbuca vs Suboxone,” and more).
Quick disclaimer: This article is for education only and is not medical advice. Opioids can cause serious harm, including addiction, overdose, and death. Use Belbuca only as prescribed and under the supervision of your healthcare professional. If you think you or someone else is experiencing an overdose (very slow or stopped breathing, extreme sleepiness, blue lips), call emergency services immediately.
What Is Belbuca?
Belbuca is the brand name for buprenorphine buccal film. Each individually sealed film is designed to adhere to the buccal mucosa (the inner cheek) and dissolve over about 30 minutes. Belbuca is used only for chronic pain that requires continuous opioid treatment and is not appropriate for occasional or short-term pain.
Strengths and Dosing Frequency
Belbuca films come in the following microgram (mcg) strengths, dosed every 12 hours (twice daily):
- 75 mcg
- 150 mcg
- 300 mcg
- 450 mcg
- 600 mcg
- 750 mcg
- 900 mcg
Never cut or split a film. Use exactly the strength your prescriber chooses.
How Does Belbuca Work?
Buprenorphine binds strongly to μ-opioid receptors and partially activates them, decreasing transmission of pain signals in the brain and spinal cord. Three features set it apart:
- Partial agonism – Provides analgesia with a plateau in respiratory depression at higher exposures than full opioids. This doesn’t remove risk, but it changes the risk profile.
- High receptor affinity – Buprenorphine can displace other opioids from receptors. If started too aggressively in someone taking high-dose full-agonist opioids, this may trigger withdrawal; that’s why conversions are done carefully.
- Long duration – Adheres and releases medicine gradually, allowing twice-daily dosing.
When Do Doctors Prescribe Belbuca?
Belbuca may be chosen for patients who:
- Have chronic musculoskeletal pain (e.g., back pain, osteoarthritis) not controlled with non-opioids and non-pharmacologic therapy.
- Need continuous opioid therapy but may benefit from buprenorphine’s ceiling effect on respiratory depression relative to full agonists.
- Do not tolerate other opioids due to side effects.
- Prefer a non-swallow, non-injectable route of administration.
Not for: intermittent pain, acute postoperative pain, migraine “as-needed” use, or initial treatment of opioid use disorder (OUD) (different buprenorphine products are used for OUD under specific protocols).
Belbuca Dosage & Administration
Your dose is personalized. Do not change it without medical guidance.
Typical Starting Approach
- Opioid-naïve or non-tolerant patients: Clinicians usually start with 75 mcg once daily for the first dose, then 75 mcg every 12 hours, and adjust as needed.
- Opioid-experienced patients: The prescriber converts from your current daily morphine milligram equivalent (MME) to a conservative Belbuca dose. Because buprenorphine binds strongly, conversion is not milligram-for-milligram. The goal is to prevent withdrawal while avoiding oversedation.
Titration (Careful Dose Increases)
- Doses may be increased in 150-mcg increments (e.g., 150 → 300 → 450 mcg every 12 hours), no more often than every 4 days, based on pain relief, function, and side effects.
- Maximum recommended dose: 900 mcg every 12 hours.
Step-by-Step: How to Apply the Buccal Film
- Wash and dry your hands.
- Open one blister just before use. Do not pre-open or cut films.
- Moisten the inside of your cheek with your tongue or a sip of water (then swallow).
- Place the yellow-striped side against the inside of your cheek.
- Press and hold the film in place with a clean finger for 5 seconds to ensure adhesion.
- Let the film dissolve completely (about 30 minutes). Do not chew, swallow, or move it.
- Avoid eating or drinking until the film is fully dissolved.
- Alternate cheeks with each dose to reduce irritation.
- Dispose safely of the empty pouch and any used film backing—keep out of reach of children and pets.
If a film falls off before it fully dissolves, place a new film in the other cheek and inform your prescriber for guidance.
Side Effects of Belbuca
Most side effects are dose-related and often improve as your body adjusts. Call your clinician if symptoms are severe or persistent.
Common (generally mild to moderate)
- Nausea, vomiting, constipation
- Headache
- Dizziness or drowsiness
- Mouth irritation (redness, numbness, or tingling where the film sits)
- Dry mouth
- Sweating, itching
Serious (seek medical help immediately)
- Breathing problems (slow or shallow breathing), extreme sleepiness, difficulty waking up
- Allergic reaction (hives, swelling of face or throat, trouble breathing)
- Severe dizziness or fainting
- Adrenal insufficiency (nausea, vomiting, fatigue, dizziness)
- Serotonin syndrome when used with serotonergic drugs (agitation, sweating, fast heartbeat, muscle stiffness, confusion)
Constipation prevention tip: Adequate fluids, fiber, physical activity, and a clinician-recommended bowel regimen can help.
Warnings & Precautions
Safety first. Review these points with your healthcare professional before starting Belbuca.
- Addiction, abuse, and misuse: Even when used as prescribed, opioids carry risk. Store Belbuca securely; never share it.
- Life-threatening respiratory depression: Risk is highest when starting, increasing dose, or combining with other sedatives.
- Benzodiazepines and alcohol: Do not combine Belbuca with alcohol or benzodiazepines (e.g., alprazolam, lorazepam), sleep medicines, muscle relaxants, or other CNS depressants unless your prescriber explicitly directs and monitors you.
- Switching from other opioids: Improper conversion can precipitate withdrawal. Your prescriber will plan a gradual transition.
- Liver problems: Buprenorphine is metabolized in the liver; dose adjustments and monitoring may be needed.
- Oral health: Prolonged contact with the cheek may cause mucosal irritation; alternate sides and report persistent sores.
- Pregnancy & breastfeeding: Opioid exposure during pregnancy can cause neonatal opioid withdrawal syndrome after birth. Discuss risks, benefits, and alternatives with your clinician. Buprenorphine passes into breast milk; weigh benefits and monitor the infant for excessive sleepiness or breathing problems.
- Driving and operating machinery: Until you know how Belbuca affects you, avoid driving or hazardous tasks.
- Naloxone: Ask your clinician about keeping naloxone at home for emergency treatment of opioid overdose; teach family members how to use it.
Drug & Product Interactions
- CNS depressants (benzodiazepines, other opioids, alcohol, sedative-hypnotics): markedly increase the risk of respiratory depression and overdose.
- Serotonergic medications (SSRIs/SNRIs, MAOIs, triptans, linezolid, St John’s Wort): increase risk of serotonin syndrome; monitor closely.
- CYP3A4 inhibitors/inducers (e.g., clarithromycin, ketoconazole, ritonavir vs. rifampin, carbamazepine): may raise or lower buprenorphine levels; dose changes and monitoring may be required.
- Mixed agonist/antagonist opioids (pentazocine, nalbuphine, butorphanol): can reduce analgesia or precipitate withdrawal.
- Suboxone®/Subutex® and other buprenorphine products: Do not combine unless your prescriber has designed a plan. These are formulated for OUD; Belbuca is for pain.
Always provide a complete list of prescriptions, OTC medicines, and supplements to your healthcare team.
Belbuca vs. Other Options
Belbuca vs. Transdermal Patch (e.g., buprenorphine patch)
- Belbuca is twice-daily buccal dosing with strengths from 75–900 mcg.
- Patches deliver lower, steady buprenorphine doses over 7 days; they may suit some patients who prefer once-weekly application.
- Choice depends on prior opioid exposure, dose needs, skin tolerance, and lifestyle; your clinician will decide which is most appropriate.
Belbuca vs. Suboxone (buprenorphine/naloxone)
- Belbuca is designed and labeled for chronic pain.
- Suboxone is designed and labeled for opioid use disorder; its naloxone component discourages misuse by injection.
- They are not interchangeable without a specific medical plan.
Cost, Coupons & Generic Status
- Belbuca is a brand product. Insurance coverage varies and often requires prior authorization.
- Many pharmacies and manufacturers provide copay cards or savings programs for eligible patients.
- Ask your pharmacist about discount programs and price comparison tools to locate the best cash price in your area.
(Note: Pricing and availability change frequently; check with your pharmacist for current information.)
Practical Tips for Safe Use
- Use the smallest effective dose for the shortest duration needed to meet treatment goals.
- Do not take extra films or combine with other sedatives unless directed.
- Keep films in their original blisters; store at room temperature, dry, and out of sight of children and pets.
- Missed dose: If you miss a dose, apply it as soon as you remember unless it’s nearly time for your next dose. Don’t double up.
- Stopping Belbuca: Do not stop suddenly. Your clinician will provide a gradual taper to reduce withdrawal symptoms.
- Dispose properly: Ask your pharmacist about drug take-back options. If unavailable, follow the FDA’s recommended disposal steps for opioids.
Frequently Asked Questions (FAQs)
1) What are the usual Belbuca doses like 150 mcg and 300 mcg used for?
Doses are individualized. Many people start at 75–150 mcg every 12 hours, then titrate in 150-mcg steps (e.g., 300 mcg, 450 mcg) based on pain relief and tolerance. The maximum is 900 mcg twice daily.
2) How long does Belbuca take to work?
Some patients notice improvement after the first few doses. Full effect is typically assessed after several days at a stable dose. Dose adjustments are made no more often than every 4 days.
3) Can I eat or drink with the film in my mouth?
It’s best to wait until the film fully dissolves (about 30 minutes) before eating or drinking. This helps ensure the full dose is absorbed.
4) Is Belbuca addictive?
All opioids—including buprenorphine—carry the risk of addiction, abuse, and misuse. Careful selection, close monitoring, and the lowest effective dose help reduce risks.
5) What if I’m switching from another opioid?
Do not convert on your own. Your prescriber will design a plan that may lower your existing opioid dose and select a conservative Belbuca dose to avoid withdrawal and oversedation.
6) Can Belbuca be used in people with sleep apnea or lung disease?
Use requires extra caution. These conditions increase the risk of breathing problems. Your prescriber will weigh risks versus benefits and may suggest alternative therapies.
7) Is there a Belbuca generic?
As of now, Belbuca is branded. Generic availability varies by region and over time. Ask your pharmacist about current options and any cost-savings programs.
8) Belbuca vs. buprenorphine patch—how do I choose?
Both may be used for chronic pain but differ in dose ranges, application sites, and frequency (twice daily vs. once weekly). The decision depends on your pain pattern, prior opioid exposure, medical conditions, and preferences.
9) Can I use Belbuca if I’m pregnant or breastfeeding?
Opioid use during pregnancy may lead to neonatal opioid withdrawal syndrome. If you are pregnant, planning pregnancy, or breastfeeding, discuss all options and monitoring plans with your clinician.
10) Should I keep naloxone at home?
Yes—many guidelines recommend having naloxone available for anyone taking opioids. Ask your clinician or pharmacist about getting naloxone and how household members can use it.
Final Thoughts
Belbuca (buprenorphine buccal film) can be a valuable option for chronic, severe pain that requires continuous opioid therapy and hasn’t responded to other treatments. Its buccal delivery, twice-daily schedule, and buprenorphine’s unique pharmacology make it different from full-agonist opioids, but serious risks remain—particularly overdose and dependence when misused or combined with sedatives.
To get the best—and safest—results:
- Work with your clinician to set clear goals for pain relief and function.
- Use exactly as prescribed; never share your medication.
- Avoid alcohol and sedatives unless your prescriber has a plan and is monitoring you.
- Store securely and dispose properly.
- Seek help immediately if you notice signs of overdose or severe side effects.
When used thoughtfully and monitored closely, Belbuca can help certain patients reduce pain and improve daily function while prioritizing safety.

Leave a Comment